CPAP therapy is THE standard therapy for obstructive sleep apnoea – but what exactly does it do? In this article, we explain how CPAP works, the components that make up a CPAP system, what you need to look out for in daily use, and what alternatives are available.
How does CPAP therapy work?
With obstructive sleep apnoea, the muscles in the throat area become limp during sleep. The tongue can fall back or soft tissue in the throat area can collapse, blocking the airways. This causes dangerous breathing stops.
CPAP (Continuous Positive Airway Pressure) therapy prevents this from happening: The CPAP device generates a constant flow of air with positive pressure, which is guided into the airways via a mask. This pressure keeps the airways open – in a similar way to a balloon being inflated. This reduces the breathing stops so successfully that — in a best-case scenario — they will stop altogether. CPAP therapy has been the standard treatment for obstructive sleep apnoea for many years, as it’s extremely effective.
A typical CPAP system consists of three main components:
- CPAP device – the pump that generates the flow of air with positive pressure
- Hose – connects the device and mask
- Mask – has direct contact with the face and guides the positive pressure into the airways
Important: CPAP does not cure sleep apnoea, it treats the symptoms. The therapy must be used every night as long as sleep apnoea is still present.
CPAP, APAP or BPAP? – An overview of the three technologies
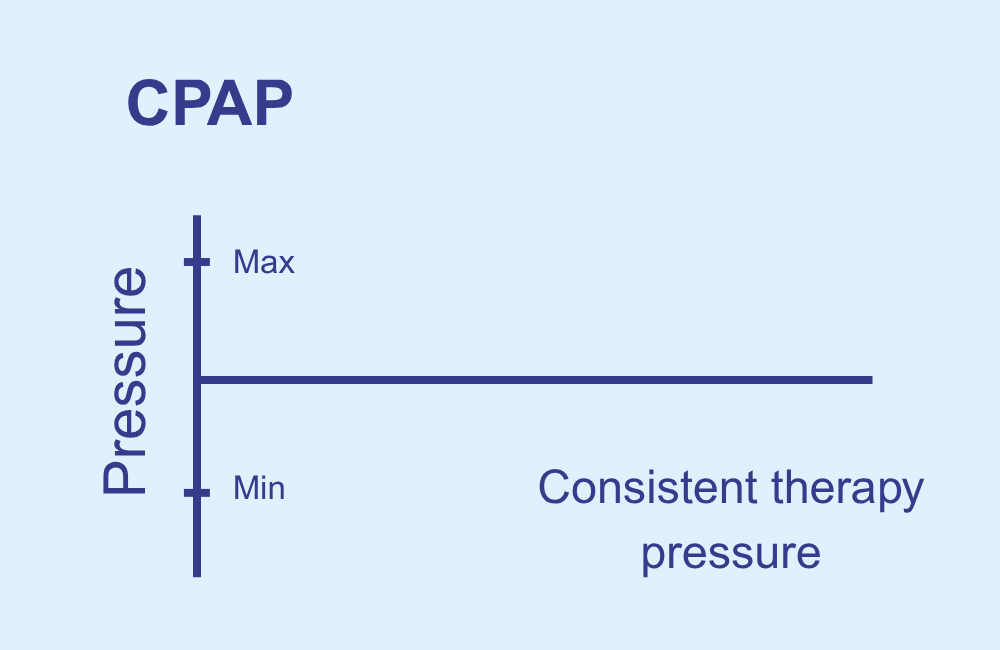
1. CPAP (Continuous Positive Airway Pressure):
The pressure is constant and preset. It’s simple, but inflexible – as breathing stops don’t occur with a regular rhythm. This technology doesn’t take into account the actual frequency of the breathing stops. There is a major disadvantage of this: Breathing stops don’t occur with a regular rhythm every hour; sometimes there will be more, sometimes fewer. The device often uses too much or too little positive pressure, which can have a significant impact on the effectiveness and comfort of the therapy.
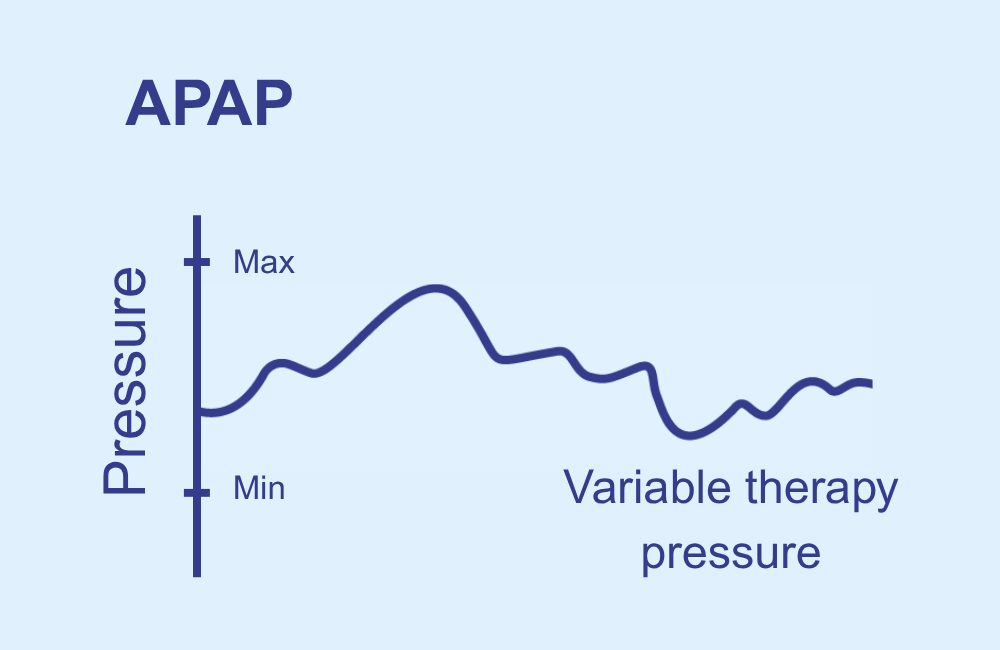
2. APAP (Automatic Positive Airway Pressure):
These devices dynamically adapt the pressure to the current sleep situation – depending on breathing patterns, resistance and any breathing stops. A lot of people therefore find APAP more comfortable, as the pressure is not consistently high, but fluctuates within a preset minimum and maximum pressure range and automatically adapts to the patient’s individual needs.
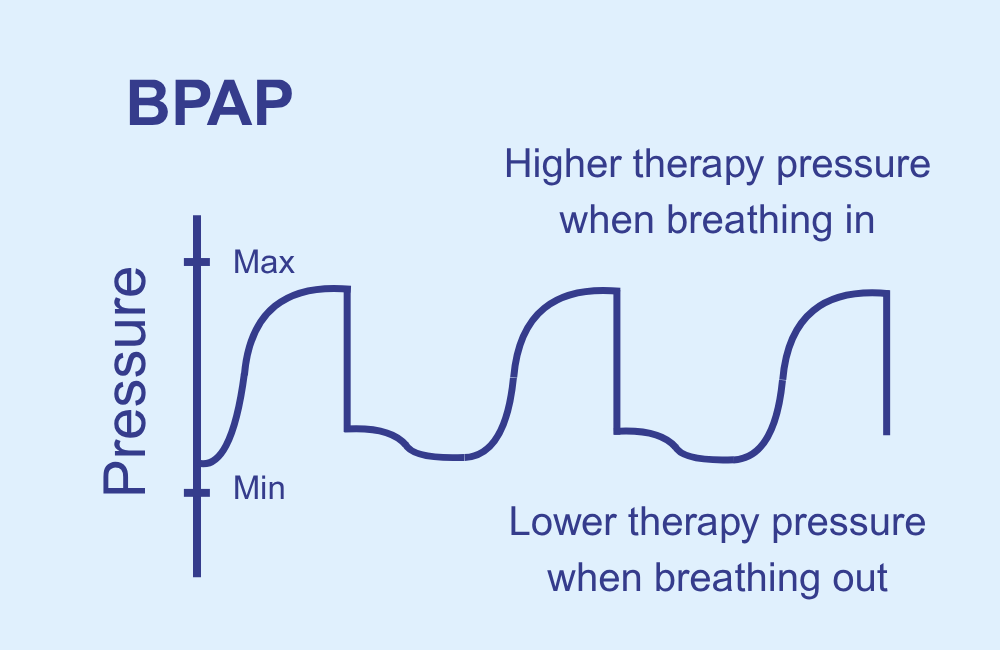
3. BPAP (Bilevel Positive Airway Pressure):
These devices have two different pressure levels: more pressure when breathing in, less pressure when breathing out. This makes breathing a lot more pleasant – especially if a high pressure is needed or in the case of COPD or central sleep apnoea. However, BPAP devices are usually much more expensive than APAP or CPAP devices.
It’s important to be aware that in everyday language, the term ‘CPAP’ is usually used as an umbrella term for the three fundamentally different positive pressure technologies. With modern APAP devices, the doctor can use the Clinical Menu to define whether the device should run in CPAP or APAP mode. There are therefore two different technologies in one device.
The key functions of modern CPAP devices
Manufacturers such as ResMed, Philips or Löwenstein offer compact, lightweight and quiet APAP and CPAP devices. The noise levels of these devices are between 33 to a maximum of 37 decibels on average. By way of comparison, a modern computer fan running on low has a noise level of 25 to 40 decibels, while a modern fridge emits 30 to 45 decibels.
Almost all CPAP devices have five practical core functions that are very important for efficacy and comfort and that patients are able to access too:
- Mask test: checks the fit and leak-tightness of the mask. The device builds up the full therapy pressure for a short period to test whether any leaks occur.
- Ramp function: the pressure gradually increases to the target value over a preset time (usually 30-45 minutes) as the patient falls asleep, in order to make the adjustment to the air flow more comfortable. The ramp time and the starting therapy pressure can usually be individually adjusted.
- Humidifier: humidifies the air in order to prevent dryness in the nose and throat (is already integrated in devices such as the Philips Dreamstation 2, and has to be retrofitted in other devices). The humidifier is filled with water, which is heated by a heater plate to create humidity. The flow of air generated by the device is then routed via this water chamber and moistens the respiratory air.
- Pressure relief: slightly reduces the pressure during exhalation, for easier exhalation. However, these pressure drops are not as marked as those in a BPAP device, which works with two different pressure levels. The name of this expiratory aid differs depending on the manufacturer, e.g. EPR in ResMed devices or FLEX in Philips devices.
- Reporting functions & apps: these show how successful the therapy has been and provide tips on improving therapy. In addition to the simple reporting functions of the devices themselves, some manufacturers also offer apps that provide comprehensive tips and coaching. These are intended to contribute to the effectiveness of the therapy and to improve commitment to therapy.
Breathing hose – heated or unheated?
CPAP hoses are usually 1.80 m long and consist of a standardised rubber sleeve (with an outer diameter of 22 mm and an inner diameter of 19 mm) and a centre section. The centre section is available in two different versions: 15 mm inner diameter and 19 mm inner diameter.
Note: Hoses with a 15 mm inner diameter are more flexible and are becoming increasingly widespread.
There are two types of hoses:
- Unheated: standard version
- Heated: with an integrated heating wire (25–30 °C) that prevents condensation (known as rainout) and heats the air to a pleasant temperature
CPAP mask – crucial for comfort and therapy success
The mask is the interface to the body – and often the biggest challenge, as it needs to fit snugly but still be comfortable. A distinction is made between nasal masks and full-face masks.
1. Nasal masks
A nasal mask is recommended as standard for those starting out with CPAP therapy. This is the mask that is worn by the majority of CPAP users, and has three major advantages compared to full-face masks. Less skin contact means less risk of skin irritations, there’s no claustrophobic feeling of being closed in as the mouth remains free, and there are fewer leaks.
Nasal masks are split into three sub-categories:
- Classic nasal masks are characterised by a triangular mask cushion that covers the area from the tip of the nose to the top lip. Older designs also have forehead support (e.g. ResMed Mirage FX), but newer designs do not (e.g. ResMed AirFit N20).
- Nasal pillow masks use small soft pads that look like nose plugs. They are inserted directly into the nostrils and seal the nose from the inside with the nasal plugs (e. g. AirFit P10)
- Minimal contact masks have a flat cushion underneath the nose. This seals the nostrils from below, but does not use nasal plugs. The air flow is fed in either from below just like with classic CPAP masks (e.g. AirFit N30) or from above via the side frame (e.g. DreamWear Nasal).
2. Full-face masks
This type of mask is used for patients who sleep with an open mouth. Because these masks also cover the mouth, they are – unlike purely nasal masks – able to ensure that the required positive pressure is built up and actually gets to the airways. They are also a common choice for when patients have a stuffy nose or need a very high therapy pressure.
Full-face masks can be divided into two sub-categories:
- Classic full-face masks have a triangular shape that covers the bridge of the nose (e.g. AirFit F20). They often have a forehead support (e.g. F&P Simplus) and are particularly suitable for very restless sleepers, who need a stable mask.
- Modern, reduced full-face masks keep the bridge of the nose free and have less contact area (e.g. AirFit F40). They are better for sensitive skin, side-sleepers and people with claustrophobia.
What are the alternatives to CPAP therapy?
Although CPAP therapy is very effective, a lot of patients struggle with compatibility issues. One particularly common reason for these issues is that the patient isn’t getting on well with the mask. A recent study from Greece (2024) found that the therapy discontinuation rate after 12 months is around 40%.
Several alternatives to CPAP therapy have therefore become established over recent years. These include:
1. Mandibular advancement devices
A mandibular advancement device is also known as a snoring mouth guard, and pushes the lower jaw forwards together with the base of the tongue. This keeps the airways clear. This therapeutic approach is now recognised as an alternative to CPAP therapy in several European countries. In cases of mild to moderate sleep apnoea, the costs of mandibular advancement devices may even be covered by health insurance providers if certain conditions are met.
2. Positional therapy
Positional therapy is suitable for positional obstructive sleep apnoea, i.e. when breathing stops primarily occur when the patient is sleeping on their back. The idea behind positional therapy is that the body is moved into a side position via physical aids (e.g. somnipax shirt) or active training systems (e.g. somnipax belt), as the base of the tongue can no longer slip back into the throat in this position. This approach is scientifically recognised and supported by studies.
3. Tongue pacemakers (HGNS)
A tongue pacemaker is a small implanted system that stimulates the tongue nerve (hypoglossal nerve) in a targeted manner so that the tongue does not fall back into the throat during sleep. A sensor detects the breathing rhythm; on inhalation, the device sends gentle impulses to the nerve via an electrode. The efficacy of these systems is well-documented, particularly for patients with moderate to severe sleep apnoea who do not tolerate CPAP therapy. Unlike the other therapy options, this system treats the cause of sleep apnoea.
Summary
CPAP therapy is the standard therapy for the treatment of obstructive sleep apnoea. It is extremely effective, provided that the mask fits, the device settings are correctly adjusted and the therapy is comfortable. Modern devices, innovative mask models and comfort products such as heated hoses make these therapies significantly more pleasant to use than they were a few years ago.
If you cannot tolerate CPAP, there are other alternative therapies such as mandibular advancement devices, positional therapy or tongue pacemakers, depending on the cause of your snoring or sleep apnoea and the level of severity.
You should always consult your physician before changing therapy method in order to check whether the desired alternative is suitable for your specific situation.
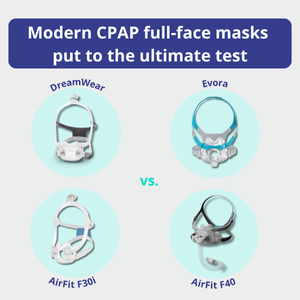
Modern CPAP full-face masks put to the ultimate test
When it comes to CPAP therapy, choosing the right mask is crucial for a restorative night’s sleep. We’ve put the most popular reduced full-face masks that cover the mouth and nose to the test for you.
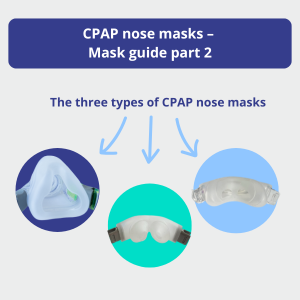
The three types of CPAP nasal masks
Choose between the three different types of nasal masks, namely classic nasal masks, nasal pad masks and minimal contact masks.
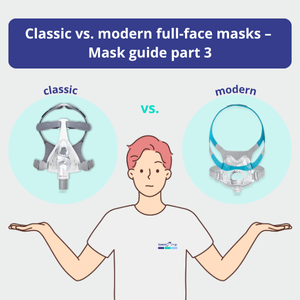
“The right CPAP mask” practical guide: Classic vs. modern CPAP full-face masks
Know that you need a full-face mask but unsure how to choose the right one? The “Choosing the right CPAP mask” practical guide is all about choosing between the two different types of full-face masks, namely the classic full-face masks and the modern, reduced full-face masks.
Dr. Daniel Grätz is the Managing Director of health.On Ventures GmbH, one of Germany’s leading online providers of snoring mouth guards, and has been providing customers with advice about these devices for many years.