Do you suffer from side effects as a result of wearing a sleep apnoea mask? Then you are not alone! Dry mouth, pressure sores and the like are a great physical and psychological burden, which make wearing a sleep apnoea mask increasingly difficult. Unfortunately if a sleep apnoea mask is not used regularly, the therapeutic effect is of no value, and in the end you it doesn’t do anything to improve your health. Today, however, there are numerous treatment options available in addition to the sleep apnoea mask. In this article we inform you of alternative therapeutic options available to treat your sleep apnoea.
If you would still like to get an overview of suitable CPAP mask types first, you can find an overview of all CPAP masks here.
According to Studies about 65% of people who use sleep apnoea masks suffer from dry mouth, which is the most common side effect. In addition, about 50% of all patients suffer from pressure sores, pain and/or allergies caused by the mask. In addition to the classic sleep apnoea mask, there are both invasive and non-invasive alternative methods for treating sleep apnoea. The therapeutic measure that is most suitable for you is dependent, among other things, on the severity of your sleep apnoea and should only be be decided upon after consulting your doctor.
Non-Invasive Therapeutic Alternatives
Behavioural Therapy
A change in lifestyle is the cornerstone of successful sleep apnoea treatment. Cases of mild OSAS can be treated in this way, as an alternative to the sleep apnoea mask. In all other cases, a change in lifestyle will most likely contribute to an improvement of symptoms.
Weight Loss
Being overweight is one of the main causes of snoring. According to a US study the risk for OSAS increases in correlation with obesity. Thus, about 40 percent of moderately overweight and up to 90 percent of severely overweight people are affected by OSAS. The additional fat deposits are not only deposited in the abdomen, bit in the throat area too, and hamper breathing. In addition to the usual areas, fat cells also accumulate in the throat and pharynx and obstruct the airway. Apnoea develops as a result. Therefore a healthy diet and sports program should be followed. Once you have reached your ideal weight, it is crucial to maintain it, otherwise, there is a high probability that sleep apnoea will occur again.
Abstaining from Alcohol and Nicotine

Alcohol and nicotine should be avoided for at least four hours before you go to bed. Alcohol has a relaxing effect on the muscles in the throat area, which results in a higher prevalence of snoring and apnoea. Smoking is also one of the risk factors for OSAS. However, due to a lack of medical evidence, a clear connection between the two has not yet been fully established.
Abstaining from Certain Medications

Medications for the treatment of anxiety and sleep disorders often contain certain active ingredients which have a relaxing effect on the muscles and can thus lead to apnoea. These include medications with the following active ingredients; benzodiazepines, barbiturates and antihistamines. Studies have shown a relation to these substances and a decrease in blood oxygen saturation levels, which in the long term can cause damage to organs and disturb the metabolic process and can lead to serious secondary diseases. More large-scale, long-term studies are needed to investigate the effects of tranquilisers on people with sleep apnoea.
Sleep Hygiene

In general, there are some basic rules that you can follow for a healthy and restful sleep. These include topics such as diet, exercise, sleeping environment, etc. Read more about healthy sleep hygiene in our sleep tips.
Positional Therapy
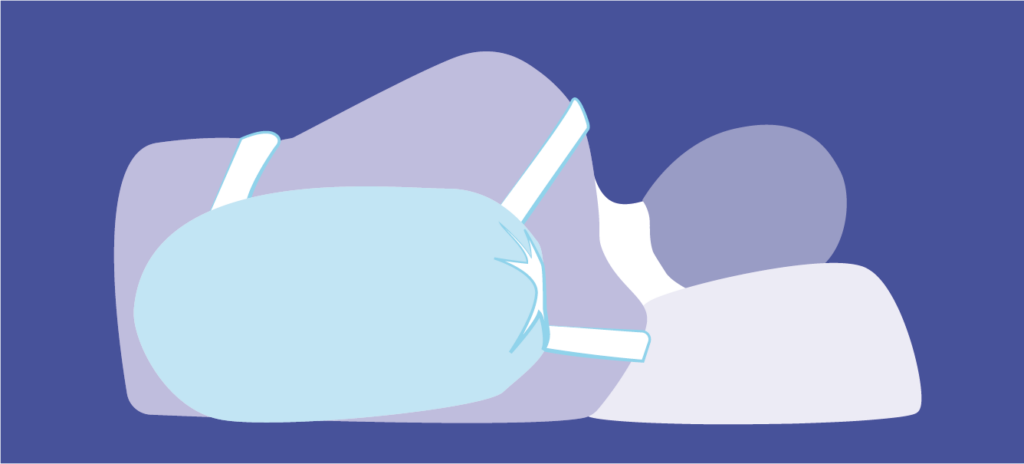
Your sleeping position plays a significant role in whether you snore or not. Sleeping on your back contributes to the fact that gravity causes the back part of the tongue, the so-called base of the tongue, to slide backward into the back of the throat and obstruct the airway. This leads to snoring and possibly apnoea.
One treatment option for OSAS, associated with tongue-based snoring, is positional therapy. This includes products such as anti-snoring pillows, ant-snoring T-shirts or electronic positional therapy belts. These, so-called, positional therapy aids are designed to prevent you from rolling onto your back thanks to padding or inserts such as inflatable cushions. The aim is to prevent you from sleeping on your back, which is the cause of tongue-based snoring and to facilitate you sleeping on your side or stomach.
CPAP pillows with side cut-outs for the mask are also a special aid for CPAP users, reducing pressure on the face and making it easier to lie on your side.
If positional therapy is consistently practiced for a few months, you become conditioned to sleeping on your side. It is therefore quite possible you may then no longer need the therapeutic aid and as you are now conditioned to automatically sleep in this position. It remains critical to note that there is a chance that your quality of sleep could suffer as a result. In addition, many people experience apnoea in other sleeping positions as well. We can provide you with more detailed information about positional therapy aids.
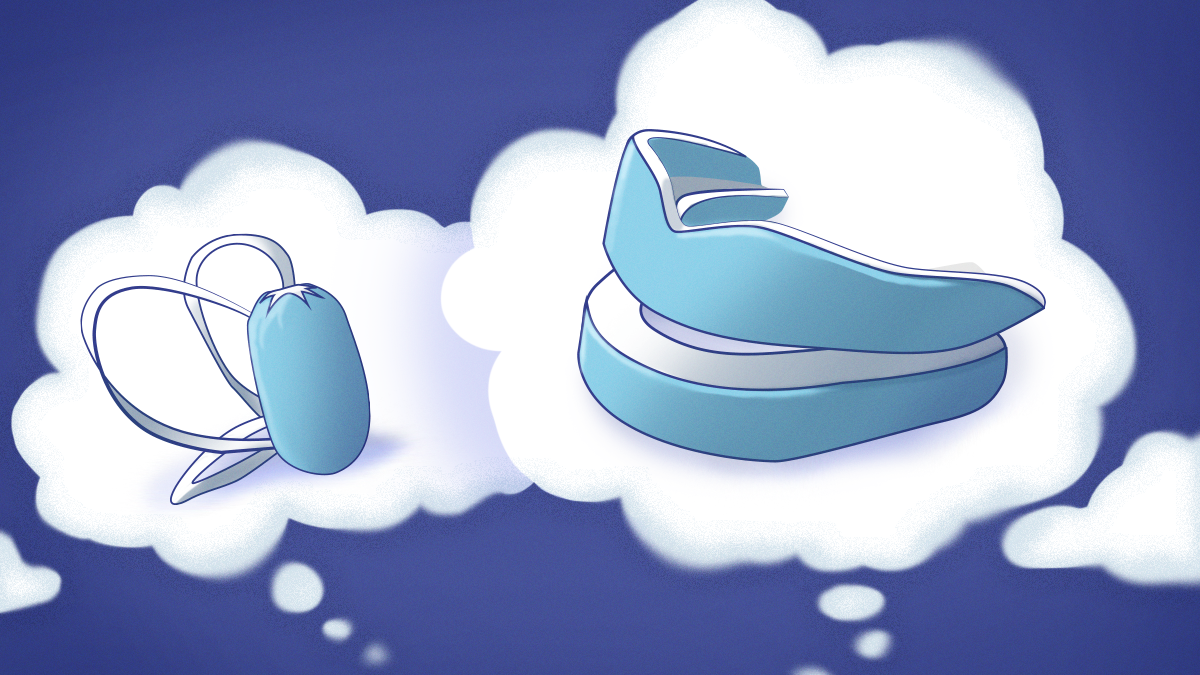
Mandibular Advancement Devices

In cases of mild-to-moderate sleep apnoea, mandibular advancement devices (MADs), are often the preferred choice and as an alternative to a sleep apnoea mask. They effectively prevent tongue-based snoring by moving the lower jaw (mandible) and the base of the tongue, forward by a few millimetres (advancement). This prevents the base of the tongue from sliding backward into the back of the throat and obstructing the airways. MADs are available in customisable or ready-made versions. The models that are made to measure by a dentist or dental technician are considerably more expensive than those sold over the counter.
Approximately â of MAD users suffer from increased salivation, pain in the temporomandibular joint and dry mouth in the beginning. In the vast majority of cases, however, the side effects disappear after an acclimatisation period of one month. In general, care must be taken to ensure that the teeth and gums are healthy, otherwise it can lead to misalignment of the teeth, in the worst case. Regular dental check-ups are advisable. Here you can find detailed information about mandibular advancement devices.
Medication
At the moment there are no suitable pharmaceuticals on the market, for treating sleep apnoea, which meet the criteria of evidence-based medicine.
Invasive Treatment Options
If non-invasive treatment methods are unsuccessful, the only remaining option is to perform a more invasive therapeutic procedure, i.e. surgery. The aim of such an operation is always to eliminate the cause of the apnoea. Depending on the severity of the sleep apnoea and the characteristics of the upper respiratory tract, surgery is performed on the problematic region e.g. the nose, the palate, the tongue or the base of the tongue.
Subsequently, different methods exist. These include jaw corrections and nose operations to improve nasal breathing. In addition, to surgical procedures for the tightening of the soft palatal tissue (uvulopalatopharyngoplasty), when the small distance between the back of the throat and the soft palate causes breathing difficulties, or surgery to remove the uvula. In the field of tongue surgery, reducing the volume of the base of the tongue was long considered the solution. This method is now obsolete. Instead, in recent years other therapy alternatives have emerged. These include tongue base implants and tongue pacemakers (hypoglossal nerve stimulators) to stimulate the muscles in the base of the tongue. Both of which aim to prevent the base of the tongue from sliding backward.
We would like to briefly describe two of these invasive, alternative therapeutic approaches for the treatment of sleep apnoea.
Inspire Tongue Pacemaker
This new procedure is intended for patients with moderate-to-severe OSAS who cannot handle a sleep apnoea mask or for whom more conservative procedures do not work. In a clinical trial the Inspire System was able to reduce the apnoea phases by 68%. Daytime tiredness and snoring were also reduced. Another important requirement for the eligibility of this procedure is that the patient is not severely overweight , i.e. has a Body Mass Index (BMI) of less than 35 kg/m².
Method of Operation
The Inspire system consists of three parts that are implanted under the skin. A sensor on the chest measures the patient’s breathing rhythm and transmits this information to a small generator, which is located under the collarbone, similar to a pacemaker. From there, a thin wire leads to an electrode on the floor of the mouth under the chin.
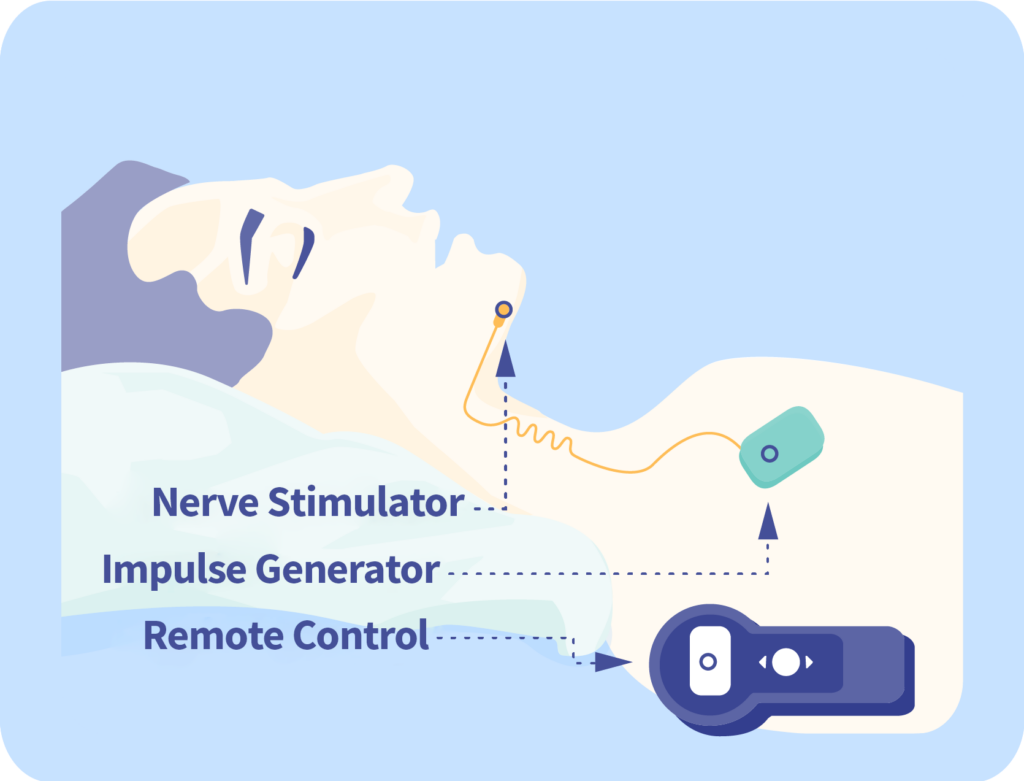
If the sensor registers a change in the breathing rhythm, the pacemaker sends a mild electrical impulse to the electrode. This stimulates the muscles in the floor of the mouth and thus prevents the tongue from obstructing the airway. In this way, the airways remain unobstructed during sleep. The system is activated with a small remote control before bedtime and switched off again in the morning.
Revent Tongue Implant
The Revent system is particularly suitable for patients whose OSAS is caused by the base of the tongue sliding backwards into the back of the throat. The device is inserted into the tongue by means of a minimally invasive procedure.
Method of Operation
The device comprises of between one to four rod-shaped implants made of elastic silicone with a loop at the end. This loop is used for healing and fixation after implantation. Prior to the operation, the implants are coated with a substance that is broken down by the body after a few weeks. As a result the rods contract and act like a splint preventing the base of the tongue from sliding backwards into the back of the throat. Due to the elasticity of the implants, normal tongue movements are not affected.


In addition to the health risks of the operation, success is not guaranteed. The higher the BMI and the starting apnoea-hypopnoea index (AHI), the lower the chances of success. There are numerous other surgical procedures available.
Note: In cases of nasal obstruction, simple aids such as nasal douches, nasal sprays or, in particular, nasal dilators can help to improve nasal breathing. Find out more about our selection of nasal dilators here.
What You Should Know Before Buying a Mandibular Advancement Device
Advice on what to look for when buying a mandibular advancement device (MAD). Different models and technical approaches explained.
What You Should Know Before Buying a Positional Therapy Aid
Advice on deciding on a positional therapy device, such as positional therapy vests or anti-snoring backpacks.

Medical Doctor, Berlin
Jan Wrede works as a medical doctor in Berlin. He studied medicine at FAU University in Erlangen-Nuremberg and Semmelweis University in Budapest. He had already written numerous scientific articles during his studies, especially on the subject of snoring.










 Welcome to SomniShop
Welcome to SomniShop